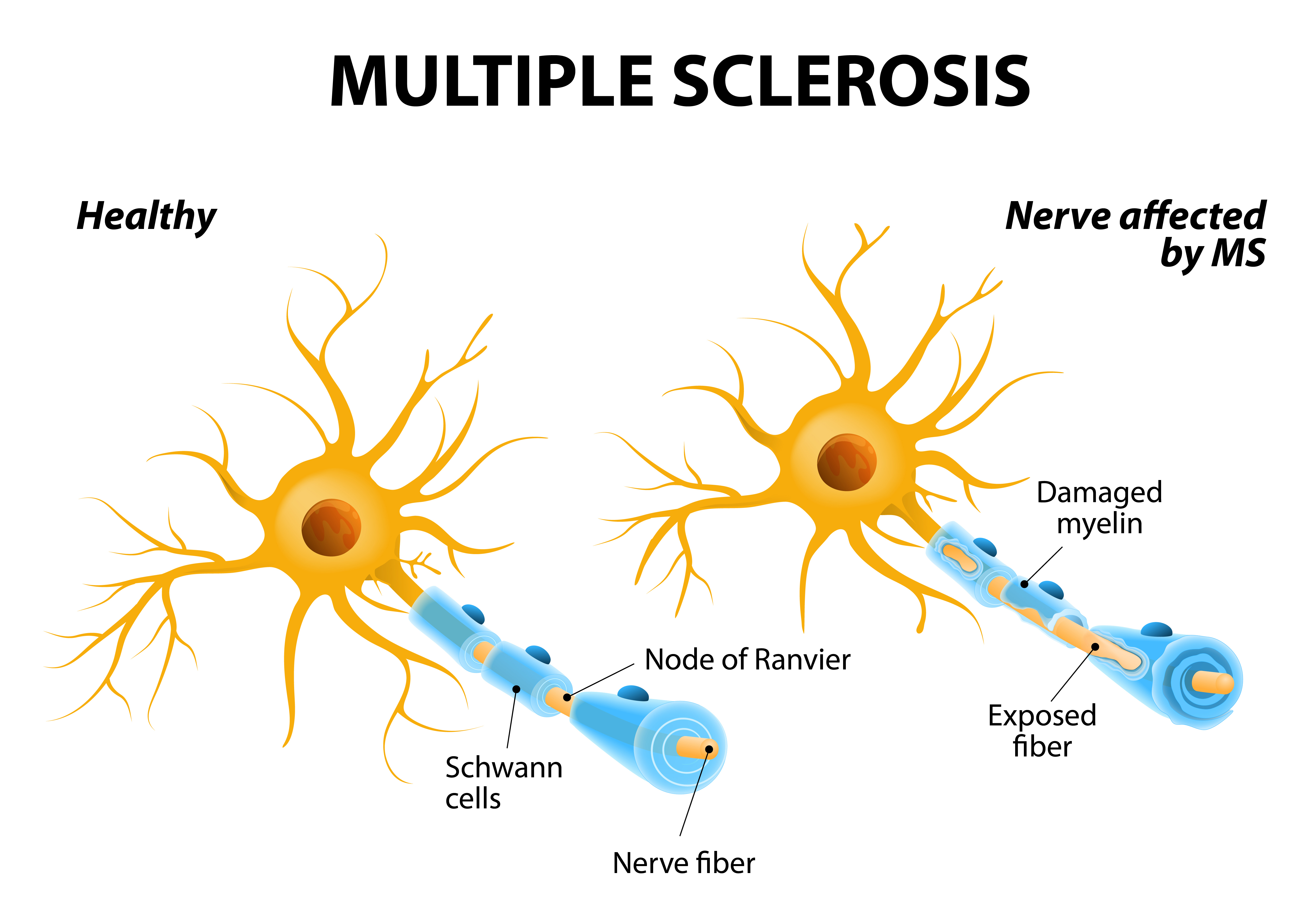
Multiple sclerosis is a complex disease, and its many patterns of progression make each case unique. Multiple sclerosis is an autoimmune disease that affects the body’s ability to send nerve signals. It occurs when your immune system attacks the myelin sheath, a protective coating on your nerve cells. The myelin sheath is like insulation on a wire. It doesn’t just protect the nerve from damage; it also keeps the signal from being lost or distorted. When your myelin coating is damaged, the nerves inside it can’t properly send signals, and the exchange of information between your body and brain is disrupted. MS also causes the immune system to attack oligodendrocytes, the myelin-producing cells that would otherwise repair the damaged sheath. When your myelin is damaged, the nerves inside it can’t properly send signals, and the exchange of information between your body and brain is disrupted.
Although no two people experience MS in the same exact way, researchers have identified 4 major types of the disease that can be used as guidelines for prognosis and treatment. To that end, MS is classified as:
- Relapsing-remitting,
- Secondary progressive,
- Primary progressive, or
- Progressive relapsing
Out of every twenty people diagnosed with MS,
- 17 have relapsing-remitting MS;
- two have primary progressive MS; and
- one has progressive-relapsing MS.
About 65%— or 11 out of 17—people diagnosed with relapsing-remitting MS will go on to develop the fourth type of the disease, secondary progressive MS.
Relapsing-remitting multiple sclerosis, or RRMS, is by far the most common form of the disease; in fact 17 out of every 20 people with MS will have RRMS at the time of their diagnosis.
RRMS usually develops at a younger age than other forms of multiple sclerosis, typically between age 20 and 50, and affects women about two to three times as often as men. RRMS is characterized by cycles of relapse and remission. During relapse, MS symptoms appear for days, weeks, or months at a time before lessening or completely disappearing during longer periods of remission.
In Secondary progressive MS, symptoms worsen continuously, even though there may be some periods of relative stability. Most people with relapsing-remitting MS will develop secondary-progressive MS at some point in their lifetime.
The transition between relapsing-remitting MS and secondary-progressive MS usually occurs 10 or more years after the initial diagnosis, though the specific boundary line between the two types is difficult to determine.
Here’s an example of the difference between the two:
- A patient who has relapsing-remitting MS might report: “Four weeks ago on Wednesday morning, I experienced a sensation of tingling and burning in my leg, it worsened over a few days, but in the weeks since then it has improved.”
- A patient who has secondary-progressive MS might say: “I don’t remember when exactly the tingling and burning in my leg started, but it has been getting worse very gradually for the past six months.”
Primary progressive MS, or PPMS, occurs when symptoms steadily worsen from the start of the disease. Symptoms may stop worsening or may even slightly improve for a while, but there are no clear remissions or relapses. About 1 out of every 10 people with MS has PPMS. PPMS affects men and women equally, and it tends to start at a later age–usually in a person’s 40s or 50s. PPMS is often the hardest form of MS to treat because the medications for relapsing MS focus on treating inflammation, which seems to be less important in this form of the disease. Progression is variable among individuals.
Progressive relapsing MS, or PRMS, is the rarest form of the disease, affecting only 1 out of every 20 people with MS. PRMS has a progressive course from onset, like PPMS, but includes superimposed acute relapses, from which there may be complete or partial recovery. Medications are available to treat inflammation and potentially slow the course of the disease, however the varying forms of MS respond to medications in different ways. There is ongoing research focusing on the treatment of progressive forms of MS, as there is currently no approved disease modifying therapy for this type of the disease. Talk to your doctor to determine which course of treatment is best for you.
MS is most commonly diagnosed in women aged 20 to 50 years. Family history of MS may raise your risk for the disease, as can some viruses, such as Epstein-Barr, the virus responsible for mononucleosis. Smoking both increases your chances of getting MS and accelerates progression of the disease. The presence of other autoimmune diseases can also increase your risk since it reflects an auto-reactive tendency, while immune regulating compounds, like the Vitamin D your body makes as a result of sun exposure, may lower your risk.
MS can be challenging, both physically and emotionally, the proper medical regimen allows many people with this disease to live normal or near-normal lives.