Sleep apnea is a potentially serious breathing disorder that affects more than 18 million Americans. If you have sleep apnea, your body stops breathing when you sleep, and you need to wake up to breathe again—creating a cycle of waking and sleeping that can impact health in significant ways. You may wake up gasping for breath, or you might stir from sleep so briefly you don’t notice waking up. Some people with severe sleep apnea may stop breathing more than 30 times in an hour of sleep.
Stopping breathing in the nighttime may sound serious, and it is. For most people, sleep apnea doesn’t stop your breathing long enough to put you at risk of immediate harm—but over the long term, sleep apnea can lead to other serious problems, including heart disease, memory lapses, and impotence. And being tired from poor sleep can get in the way of your work or your home life, or even put you at risk for a serious accident.
There are two basic types of sleep apnea:
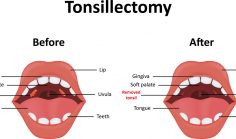
- Obstructive sleep apnea is by far the most common type. In obstructive sleep apnea, your breathing stops because something gets in the way, like your tongue or your soft palate, or the muscles in your throat relax and let your windpipe close up so that air can’t get through.
- Central sleep apnea is much less common; in central sleep apnea, your brain fails to send an important signal, and the muscles in your airways just “forget” to breathe.
Many people with central sleep apnea suffer from obstructive sleep apnea as well. Having both types at once is known as mixed sleep apnea, or complex sleep apnea syndrome. Complex sleep apnea is, in fact, more common than central sleep apnea on its own. According to one study of 223 people with sleep apnea:
- 188 people, or about 84%, had obstructive sleep apnea
- 34 people, or 15%, had complex sleep apnea syndrome
- Only 1 patient, less than ½%, had central sleep apnea alone
Regardless what type you have, sleep apnea affects the quality of your sleep and can leave you tired in the morning.