Snoring occurs when you have difficulty circulating air freely through your nose, mouth, and throat during sleep. When these passageways are restricted or narrowed, the air being forced through them causes the tissue of the palate (roof of the mouth) and throat to vibrate. The sound varies with the degree of the obstruction. The result of this turbulent airflow is the non-melodious sounds of snoring.
The first order of business is to understand the different types of snorers:
Nose snorers. Humans are hardwired to breathe through the nose as that organ is what filters and humidifies air entering our bodies—it is most common to breathe through our noses when sleeping. Nasal snoring is due to swelling in the nasal cavity (often caused by allergies) or a deviated septum. When the nasal cavity is constricted or obstructed, the air is forced through these narrow passageways, causing the tissues to vibrate and ZZZZZZZ.
Mouth snorers. Sometimes people with restricted nasal passageways breathe and thus snore through the mouth, even though the problem originates with the restricted nasal passages. Generally, those whose snores emanate from the mouth are reacting to the relaxation of soft tissue at the back of the mouth, which creates the restriction of airflow through the passageway. This restriction leads to the vibration of the soft tissues that causes the snoring.
Here is an explanation of the different soft tissues:
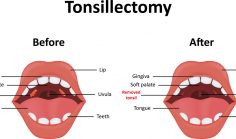
The Soft Palate. This muscle goes from the roof of the mouth to the back part of the mouth. While the soft palate is attached to the bones at the front and sides of the mouth it really is hanging free at the base of the mouth. Thus it can move forwards and backwards to open or close the connection between the nasal passageway and the mouth. When you are breathing, the soft palate moves forward to allow the passage of air. When eating or drinking it moves backward to prevent anything that is being ingested from entering the nasal cavity. For instance it allows salad and iced tea to go down your throat.
Uvula. The little ‘ball’ that hangs down at the back of the mouth is called the uvula. It helps the soft palate perform its jobs.
Tongue. As you know from a lifetime of experience, the tongue is not anchored tightly in the mouth. Rather, it freely moves around in order to aid in the tasks of swallowing and speaking.
Snoring is a Common Affliction
As anyone who snores and/or sleeps with a person who ‘saws logs’ can surmise – this affliction is common. Indeed, according to the American Academy of Otolaryngology (AAO) 45 % of normal adults are occasional snorers and 25 % suffer from habitual snoring. Snoring typically worsens with age because the muscles in the nose, mouth and throat lose tension. As the air passageway become even more easily restricted, snoring increases in frequency and volume. Perhaps this is one of the reasons of midlife marital malaise!
In all seriousness heavy snoring might be more than a nuisance to all within earshot. It can be an indication of obstructive sleep apnea. One in three men, and approximately one in five women who are habitual snorers, suffer from this malady to some degree. Obstructive sleep apnea (OSA), which causes you to temporarily stop breathing for short periods of time while you sleep, is a serious sleep disorder as well as a risk factor for health issues such as stroke, diabetes and heart disease.